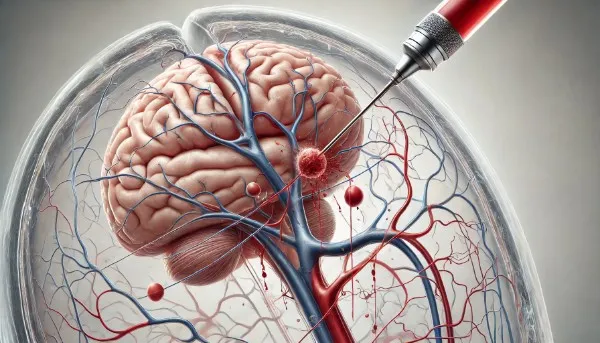
The human brain relies on an extensive network of blood vessels to sustain its optimal function. However, within this intricate vascular system, vulnerabilities arise in the form of brain vascular malformations. These anomalies can trigger serious health complications, such as hemorrhages and neurological deficits.
In the search for an effective remedy, the medical field has witnessed the rise of an innovative approach – embolization. This technique has gained prominence due to its minimally invasive nature and potential to mitigate the consequences of brain vascular malformations. It offers hope for improved outcomes and enhanced well-being for those afflicted by these conditions.
In this comprehensive blog, we will explore the effectiveness of embolization as a treatment option for brain vascular malformations.
What are Brain Vascular Malformations?
The following anomalies in the brain’s blood vessels can manifest in various forms:
- Arteriovenous Malformations (AVMs): Abnormal tangles of arteries and veins that disrupt the typical blood flow pattern.
- Cerebral Cavernous Malformations (CCMs): Clusters of dilated and irregularly shaped blood vessels.
- Dural Arteriovenous Fistulas (DAVF): Abnormal connections between arteries and veins within the brain’s dural covering.
- Capillary Telangiectasias: Tiny, dilated capillaries that may be prone to bleeding.
These malformations, although diverse, share the potential to cause health issues, such as hemorrhages, seizures, and neurological deficits. The treatment choice for these conditions is critical for both patients and healthcare professionals.
What are Some Important Global Statistics on Brain Vascular Malformations?
To grasp the gravity of brain vascular malformations, let’s consider the global statistics:
- Prevalence: Brain vascular malformations are relatively rare, with an estimated majority of 10 to 18 cases per 100,000 people.
- Hemorrhage Risk: The risk of bleeding varies depending on the malformation type. For instance, AVMs have an annual hemorrhage risk of approximately 2-4%.
- Age Distribution: These conditions can affect individuals of all ages but are often diagnosed in young adulthood.
- Health Consequences: Hemorrhages from brain vascular malformations can lead to significant disabilities and mortality.
Is Embolization a Viable Treatment Option?
Embolization, or endovascular embolization, is a minimally invasive medical procedure involving injecting an embolic material into the blood vessels to block or reduce blood flow to the affected area. This technique is primarily employed for AVMs and DAVFs in brain vascular malformations. Let’s explore the effectiveness of embolization in managing these conditions:
- a) Arteriovenous malformations (AVMs): Embolization can be used as a preoperative measure to reduce AVMs’ size and blood flow before surgical resection, making the surgery safer and more effective. In some cases, complete obliteration of the AVM can be achieved through embolization alone.
- b) Dural arteriovenous fistulas (DAVFs): Embolization is a well-established treatment for DAVFs. Closing the abnormal connections between arteries and veins can eliminate the source of abnormal blood flow.
Dr. Vikas Gupta says, “The minimally invasive nature of embolization offers patients a path to quicker recovery and improved well-being.” However, he advises that the decision be made in collaboration with a skilled medical team, considering the patient’s unique condition and overall health.
How Effective is Embolization?
Embolization has shown promising results in treating brain vascular malformations, contributing to its increasing popularity. The effectiveness of embolization can be evaluated based on several key factors:
- Hemorrhage Prevention: One primary goal of treating brain vascular malformations is to prevent hemorrhages. Embolization can effectively reduce blood flow to the malformation, minimizing the risk of rupture.
- Symptom Relief: Embolization can alleviate the neurological symptoms associated with vascular malformations, enhancing patients’ quality of life.
- Complete Obliteration: In some cases, embolization alone can lead to total obliteration of the malformation, eliminating the need for further treatment.
- Preoperative Preparation: For surgical resection of AVMs, embolization can be a valuable preparatory step. It reduces the size and vascularity of the malformation, making the surgery safer and more successful.
- Minimally Invasive: Embolization is a minimally invasive procedure, resulting in smaller incisions, shorter hospital stays, and quicker recovery than open surgeries.
Dr. Vikas notes the effectiveness of embolization in treating brain vascular malformations. He highlights its capacity to prevent hemorrhages, alleviate symptoms, and sometimes wholly obliterate the malformation.
“By reducing blood flow, embolization minimizes the risk of rupture, enhancing patient safety and well-being. Additionally, the minimally invasive procedure results in shorter hospital stays and quicker recoveries than traditional open surgeries, ” says Dr. Vikas.
Additionally, he emphasizes that each case is unique, and the decision to opt for embolization should be based on a comprehensive evaluation by a team of experienced medical professionals, considering the patient’s specific condition and overall health.
What are Some of the Risks and Considerations?
While embolization is a valuable treatment option, it is not without risks and considerations:
- Risk of Recurrence: Vascular malformations can sometimes partially recur after embolization, necessitating follow-up treatments.
- Potential Complications: Embolization can carry the risk of complications, such as stroke, embolism, or damage to normal brain tissue.
- Expertise Required: Performing embolization for brain vascular malformations requires specialized skills and expertise, emphasizing the importance of seeking treatment from experienced interventional neuroradiologists.
Thus, in neurointervention, embolization has emerged as a powerful tool in treating brain vascular malformations. Its effectiveness in preventing hemorrhages, relieving symptoms, and achieving complete obliteration has led to its increasing adoption by healthcare professionals and patients. The decision to pursue embolization should be based on a thorough evaluation of the specific malformation, the patient’s overall health, and potential risks and benefits.
In a landscape where every decision counts, the treatment choice for brain vascular malformations carries significant weight. Seeking guidance from a team of experienced healthcare professionals, including interventional neuroradiologists, is essential. Your vascular health is paramount, and the collaboration between medical experts and patients is the key to achieving the best possible outcome.
FAQs
1. How long is recovery after embolization?
Typically 1-2 weeks for light activities, but full recovery may take months.
2. Can embolization be repeated if needed?
Yes, but feasibility depends on the malformation’s response and patient health.
3. Are there lifestyle restrictions post-procedure?
Avoid strenuous activity for 4-6 weeks and blood-thinning supplements if prescribed.
4. When to seek emergency care after embolization?
For sudden severe headaches, weakness, seizures, or new neurological symptoms.
5. Is embolization covered by insurance?
Often yes, but costs vary by case—check with your provider for pre-authorization.
Explore more blogs: Does Embolization Offer a Long-Term Brain Solution?
