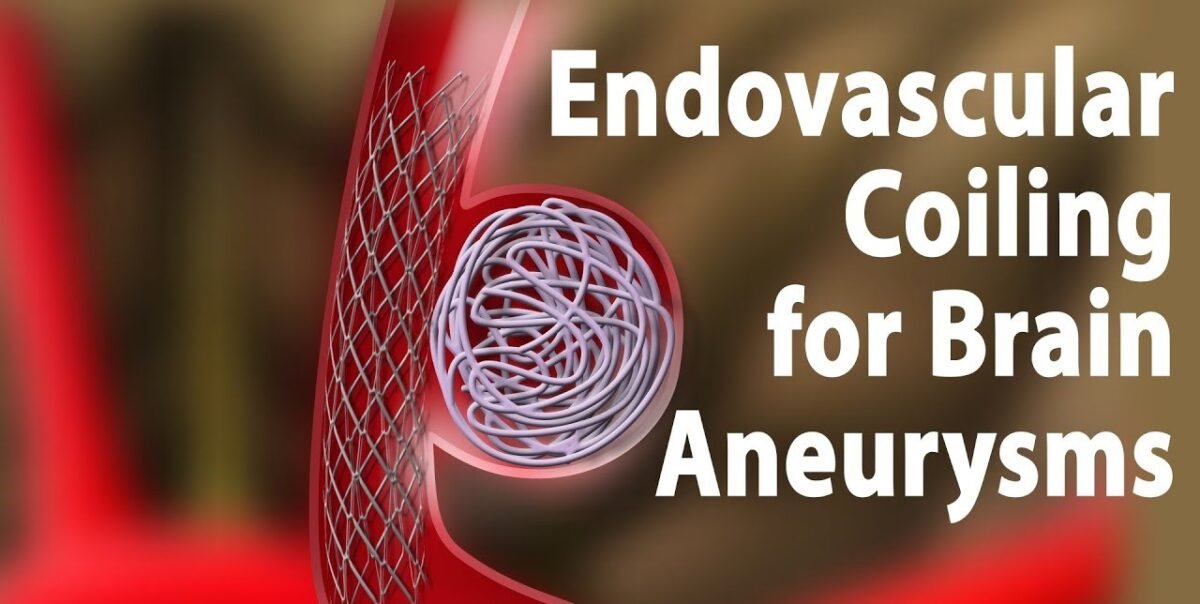
Brain aneurysms, a critical medical condition affecting millions worldwide, have been the focus of significant research and advancement. Recent global statistics reveal that approximately 6% of people are affected by brain aneurysms at some point in their lives. Among these, around 15% may experience a rupture, which can lead to severe complications or even death. Endovascular coiling, a minimally invasive technique, has emerged as a prominent treatment option for these aneurysms, offering new hope to patients and doctors alike.
This blog will delve into the details of how effective endovascular coiling is in treating brain aneurysms.
What is Endovascular Coiling?
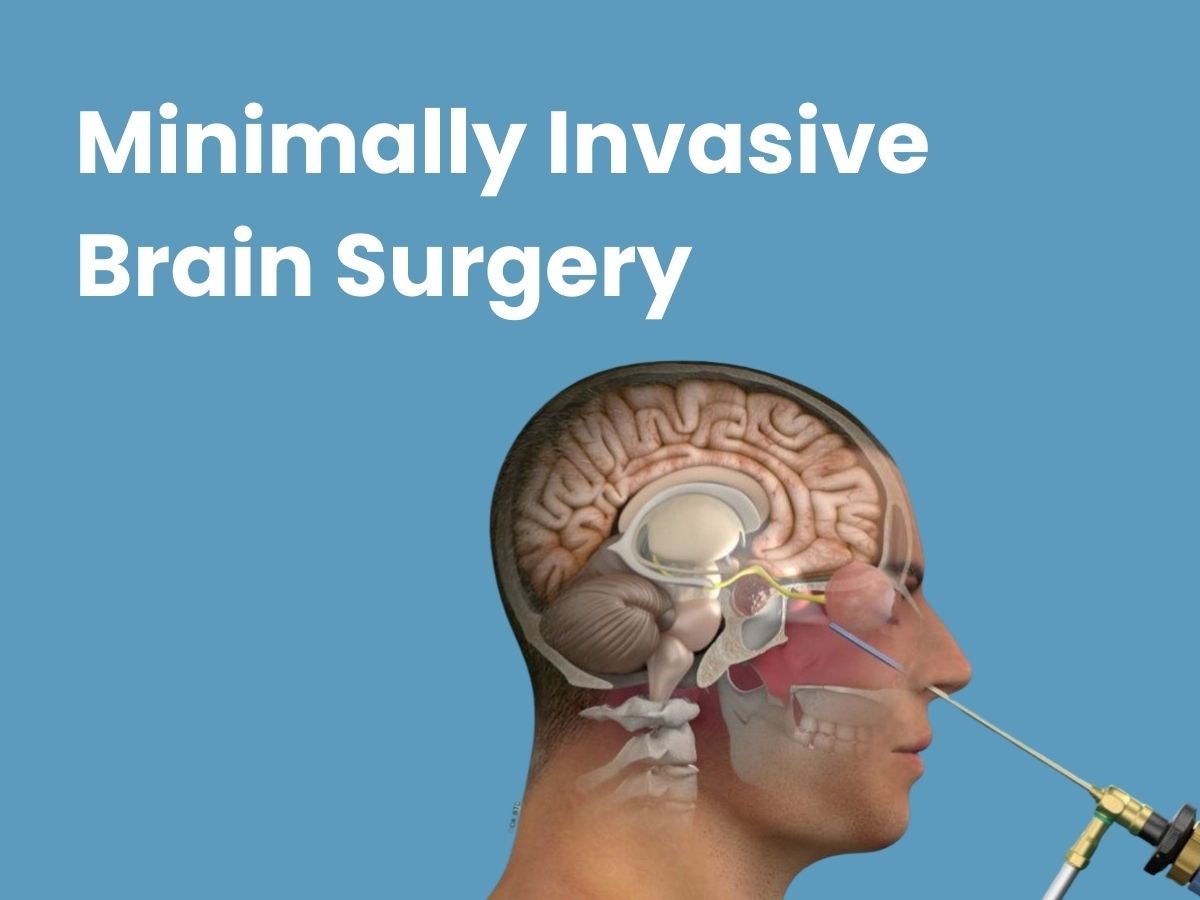
Endovascular coiling is a modern, minimally invasive procedure used to treat brain aneurysms. The procedure involves inserting a catheter through a small incision in the groin, which is then guided to the site of the aneurysm in the brain. Once in position, small coils are deployed into the aneurysm to block blood flow, thereby preventing the aneurysm from rupturing.
Dr. Vikas Gupta explains, “This technique aims to reduce the risk of bleeding and improve patient outcomes.”
How Effective is Endovascular Coiling?
Numerous studies have documented the effectiveness of endovascular coiling in treating brain aneurysms. Research shows that endovascular coiling has a success rate of over 90% in preventing aneurysm rupture, making it a highly effective treatment option. The procedure is known for its ability to reduce the risk of rebleeding and long-term complications compared to traditional surgical methods.
“Endovascular coiling is a game-changer in the field of neurosurgery,” Dr. Gupta adds. “This minimally invasive technique offers a highly effective solution for treating brain aneurysms, significantly reducing the risks associated with traditional open surgeries. By employing advanced imaging and precise catheter-based methods, we can target aneurysms with greater accuracy, leading to improved patient outcomes and faster recovery times. The ability to perform this procedure with minimal disruption to surrounding tissues has transformed how we approach aneurysm management, offering new hope to patients and setting a new standard in neurosurgical care.”
Surgical Clipping Vs. Endovascular Coiling: Which is Better?
When considering surgical clipping vs. endovascular coiling, it’s essential to evaluate the benefits and drawbacks of each approach. Surgical clipping involves placing a metal clip at the base of the aneurysm to stop blood flow. While it is a time-tested method, it requires open surgery, which carries more risks and longer recovery times.
Endovascular coiling, on the other hand, is less invasive and generally associated with fewer risks. The procedure is performed through a catheter, minimising the need for large incisions and reducing the risk of infection. Moreover, endovascular coiling allows for precise targeting of the aneurysm, potentially leading to better outcomes and fewer complications.
Dr Gupta notes, “While surgical clipping has its merits, endovascular coiling often offers a less risky alternative with quicker recovery.”
What Should You Expect During the Endovascular Coiling Procedure?
The endovascular coiling procedure is typically performed under general anaesthesia. During the procedure, a catheter is inserted through an artery in the groin and guided to the brain. Using imaging technology, the surgeon positions the catheter at the aneurysm site and deploys the coils to fill the aneurysm and prevent blood flow.
Patients can generally expect a short hospital stay and a quicker recovery compared to traditional surgical methods. Most people can return to their normal activities within a few weeks, although individual recovery times may vary.
Follow-up care often includes regular imaging to ensure the aneurysm remains secure and to monitor for any potential complications. Patients should follow their doctor’s post-procedure guidelines to ensure the best possible outcome.
One of our satisfied patients shared, “I was amazed at how quickly I recovered after my endovascular coiling procedure performed by Dr. Vikas Gupta. The process was simple, and I was back to my routine within weeks. I’m incredibly grateful for the expertise and care provided by Dr. Gupta and his team.”
Another patient said, “Endovascular coiling was a life-saving option for me. Thanks to Dr. Vikas Gupta’s minimally invasive approach, I had a shorter hospital stay and less pain than I had feared. Thanks to the fantastic medical team, I’m now living a normal, healthy life.”
What is the Cost of Endovascular Coiling in India?
One significant consideration for patients is the cost of endovascular coiling. In India, the cost of endovascular coiling can vary depending on the hospital and the complexity of the procedure.
On average, the cost of endovascular coiling in India ranges from INR 2,00,000 to INR 4,00,000. This cost may include pre-procedure assessments, the procedure itself, and post-procedure care.
Dr. Gupta highlights, “While the cost might be a concern, the long-term benefits often outweigh the initial expense.”
Conclusion
Endovascular coiling has revolutionised the treatment of brain aneurysms, offering a less invasive and highly effective alternative to traditional surgical methods. With its high success rate, shorter recovery times, and reduced risk of complications, it stands out as a preferred choice for many patients and healthcare providers.
As medical technology continues to advance, the procedure is likely to become even more refined, further improving outcomes for patients with brain aneurysms. For those facing the challenge of a brain aneurysm, understanding the effectiveness and benefits of endovascular coiling can provide reassurance and guide informed decisions about their treatment options.
FAQs
1. How long does the endovascular coiling procedure take?
The procedure typically lasts 1 to 2 hours.
2. Is endovascular coiling a permanent solution for brain aneurysms?
In most cases, it is effective long-term, though some may require follow-up procedures.
3. What are the common side effects of endovascular coiling?
Side effects can include headaches, dizziness, or nausea, which usually resolve quickly.
4. Can endovascular coiling be performed on all types of brain aneurysms?
Not all aneurysms are suitable for this procedure; the choice depends on the aneurysm’s size and location.
5. How soon can patients resume normal activities after endovascular coiling?
Most patients can return to normal activities within a few weeks.
Explore more blogs: Is Percutaneous Coiling Safer Than Surgery?
Brain tumours, characterised by abnormal growths within the brain, present a complex challenge in medical treatment. Advances in targeted therapies have significantly improved the management of these tumours, offering new hope for patients. This blog explores the latest advancements in targeted therapies for brain tumours, addressing common symptoms and costs associated with these treatments.
Brain tumours are abnormal growths of cells within the brain or surrounding tissues. They can be benign (non-cancerous) or malignant (cancerous). Tumours can originate in the brain (primary brain tumours) or spread from other parts of the body (secondary or metastatic brain tumours).
What Are Brain Tumour Symptoms?
Symptoms and severity depend on the tumour’s type, size, location, and growth rate, and they can impact brain function by pressing on or invading surrounding areas. Understanding the symptoms of brain tumours is crucial for early detection and effective treatment. Common symptoms include:
- Headaches: Persistent or worsening headaches that may be more intense in the morning.
- Nausea and Vomiting: Frequent nausea or vomiting, particularly if it occurs in the morning.
- Seizures: New-onset seizures or convulsions can be a sign of a brain tumour.
- Vision or Hearing Changes: Blurred vision, double vision, or hearing loss.
- Cognitive or Behavioral Changes: Memory problems, confusion, or personality changes.
- Weakness or Numbness: Difficulty moving parts of the body or experiencing numbness in limbs.
- Balance and Coordination Problems: Difficulty walking, balance, or coordination.
“Recognizing the early signs of a brain tumour is vital,” says Dr. Vikas Gupta. “Prompt diagnosis and targeted treatment can greatly improve patient outcomes and quality of life.”
How Do Targeted Therapies Work for Brain Tumours?
Targeted therapies aim to specifically attack cancer cells while minimising damage to surrounding healthy tissue. Recent advancements include:
- Molecular Targeted Drugs: New drugs focus on specific genetic mutations and pathways involved in brain tumour growth. For instance, drugs targeting the EGFR (epidermal growth factor receptor) mutation have shown promise in treating glioblastomas.
- Monoclonal Antibodies: These are engineered to bind to cancer cells, marking them for destruction by the immune system. Drugs like bevacizumab, which targets blood vessel growth in tumours, are examples.
- Immune Checkpoint Inhibitors: These therapies help the immune system recognise and attack brain tumour cells more effectively.
- Personalised Vaccines: Custom vaccines designed to stimulate the body’s immune response against specific tumour antigens are an exciting area of research.
Patients who have undergone these treatments have shared encouraging feedback. One patient, Anita, shared, “I never thought I’d feel hopeful again after my diagnosis. But the new targeted therapies, specially tailored for my condition, have made a world of difference.”
What are the Newest Technologies in Targeted Therapy for Brain Tumours?
Recent technological advancements enhancing targeted therapies include:
- Next-Generation Sequencing (NGS): NGS allows for comprehensive genetic profiling of tumours, identifying specific mutations and guiding personalised treatment plans.
- Tumour-Tracking Technologies: Advanced imaging and tracking methods help monitor the effectiveness of targeted therapies in real time.
- Biomarker Discovery: Research into biomarkers helps in predicting treatment response and tailoring therapies to individual patients.
“The integration of new technologies such as Next-Generation Sequencing and tumour-tracking has revolutionised the way we approach brain tumours,” Dr. Gupta explains. “These innovations allow for highly personalised treatment plans that are more effective and less harmful than traditional methods.
How Effective Are These New Treatments?
The effectiveness of targeted therapies varies based on the tumour type, genetic profile, and overall patient health. Recent studies have shown improved survival rates and quality of life for patients with targeted therapies compared to traditional treatments. However, ongoing research and clinical trials continue to refine these approaches.
What Is the Cost of Targeted Therapies for Brain Tumours in India?
In India, the cost of targeted therapies for brain tumours varies based on several factors. The type of therapy significantly impacts the price, with molecular drugs, monoclonal antibodies, and immunotherapies ranging from ₹1,00,000 to ₹5,00,000 per year. The duration of treatment also affects the overall expense, as longer and more frequent treatments can lead to higher costs.
Additionally, the healthcare setting plays a role; treatment costs may differ between private hospitals and public facilities. Insurance coverage further influences out-of-pocket expenses, with some plans covering a substantial portion of the costs. Patients must discuss financial aspects with their healthcare providers and insurance companies to understand potential costs and explore available financial assistance options.
Conclusion
In conclusion, the field of targeted therapies for brain tumours is rapidly advancing, offering promising new treatments and technologies that significantly enhance patient care. With innovations such as Next-Generation Sequencing, tumour-tracking technologies, and personalised vaccines, patients now have access to more precise and effective treatment options than ever before. These advancements are improving diagnosis, treatment efficacy, and overall patient outcomes while also aiming to reduce side effects and better manage costs.
As research continues to evolve, these therapies are expected to provide even greater benefits. Early detection and personalised treatment plans are crucial for better-managing brain tumours. Patients are encouraged to stay informed about the latest advancements and discuss their treatment options with healthcare professionals to achieve the best possible results.
FAQs
How long does it take to remove a brain tumour?
Generally, the duration of brain tumour surgery typically ranges from 2 to 3 hours, though it can vary depending on the tumour’s size, location, and complexity.
What precautions should be taken after brain tumour surgery?
Rest and avoid straining to prevent increased pressure inside your skull.
What is the most effective treatment for brain tumours?
A combination of surgery, radiation therapy, and chemotherapy is the most effective treatment for brain tumours.
How do doctors choose between radiation therapy and chemotherapy for brain tumours?
Doctors base their decision on factors like the tumor’s sensitivity to treatment, the patient’s age, and potential side effects.
What are the possible long-term effects of brain tumour treatments?
Long-term effects may include cognitive changes, hormonal imbalances, and impacts on motor function.
Explore more blogs: What Are the Benefits and Risks of Brain Tumor Surgery?